Although most people think of progressive eye conditions as primarily affecting aging adults, keratoconus is an eye condition most commonly seen in adolescents and young adults. Statistics on how common keratoconus is differs, but some studies say it develops in 50 to 200 of every 100,000 people.
If you’re in the adolescent or young adult age range, educating yourself about keratoconus may help preserve your sight. It’s essential to remain aware of the common symptoms, as the condition can cause significant vision loss.
Keep reading to learn more about whether keratoconus has any obvious symptoms.
What is Keratoconus?
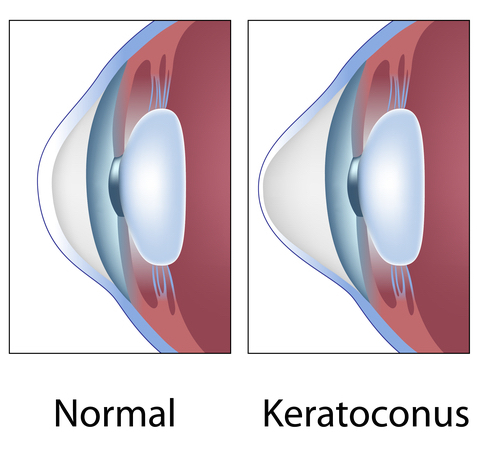
Keratoconus is a progressive eye condition, meaning it tends to develop slowly over time, often over a period of years. It occurs when your cornea, the clear dome surrounding your eye, bulges, taking on a cone-like shape.
Even slight irregularities in the shape of your cornea can cause vision problems, like astigmatism. With keratoconus, vision changes are often more severe, as the cornea’s shape changes more dramatically.
In the beginning stages of keratoconus, you may still be able to correct your vision with glasses or soft contact lenses that can fit over your cone-shaped cornea. However, as the condition progresses, your cornea can bulge so much that no contact lens can fit over it.
At that point, your vision cannot be corrected using visual aids, and you will need more intensive treatment to treat your keratoconus.
Who Is At Risk for Keratoconus?
It’s important to know your risk for keratoconus and schedule regular eye exams if you have any of the risk factors associated with the condition. Early diagnosis and treatment are crucial for preserving as much of your vision as possible and preventing the condition from progressing.
Keratoconus almost exclusively affects young people. You’re most likely to develop it in your late teens to early twenties.
It can progress into your mid-30s, but if you haven’t developed it by the time you’re 30, you’re very unlikely to. Medical experts still aren’t sure what causes keratoconus, but some conditions are often associated with keratoconus, including Down syndrome, Elhers-Danlos syndrome, asthma, and congenital eye disorders.
Frequent eye rubbing is also associated with keratoconus, although it’s unclear whether eye rubbing triggers the condition or simply accelerates it. Either way, you can lower your risk for keratoconus by not rubbing your eyes.
What Symptoms are Associated with Keratoconus?
The best way to mitigate your risk of vision loss from keratoconus is by understanding the common symptoms of the condition and attending eye exams if you start to notice them. Some symptoms associated with keratoconus include:

Worsening Vision
The primary symptom of keratoconus is blurry vision that worsens more and more over time. This can be hard to notice as your vision may worsen quite slowly.
Seeing your eye doctor at South Texas Eye Institute regularly is a good way to have your vision tested so you and your eye doctor will know if your eyesight is worsening.
Seeing Double In One Eye
Monocular double vision is when you see double, but only in one eye. Seeing double when both eyes are opened may be a sign of a neurological condition and may require further treatment, but if you see double in one eye, you should see your eye doctor as you could have keratoconus.
Light Sensitivity
If you find it hard to keep your eyes open all the way when there’s a lot of light, it could be because you’re sensitive to light. Being sensitive to light is often a symptom of keratoconus as well as a symptom of several other eye conditions.
Seeing Halos Around Lights
Keratoconus can make halos appear around lights. It can also make glare from light more intense, especially at night.
Warped Vision
Your vision becomes distorted the more your cornea bulges from keratoconus. This can make straight lines appear wavy, and objects look warped.
If you experience visual distortion, you should see your eye doctor, as it can be a symptom of certain eye conditions, including keratoconus.
When Should I See an Eye Doctor?

You should see your eye doctor if you have any of the common symptoms of keratoconus. It’s important to note that while these symptoms may be signs of keratoconus, they could be indicators of other conditions like dry eye, glaucoma, or cataracts.
Treatment options and timelines for these conditions vary, which is why it is essential to be correctly diagnosed by your eye doctor. Because keratoconus is a progressive condition, early detection is critical to maintaining your sight and avoiding more invasive treatments.
How is Keratoconus Treated?
For mild keratoconus, glasses and contact lenses can help improve vision. However, as the condition progresses, visual aids are often ineffective.
Treatments available for keratoconus at South Texas Eye Institute include:
INTACS
INTACS are tiny devices that can be inserted into the cornea to help improve your vision. They can help flatten the cornea to correct its shape and make wearing contact lenses easier.
Collagen Crosslinking
Collagen crosslinking or corneal crosslinking can help strengthen bonds between your cornea’s natural collagen fibers and surrounding proteins. This can prevent your cornea from becoming more misshapen and stop the progression of keratoconus.
Your eye doctor will place numbing eye drops and a drug containing riboflavin into your eye. Then, they will expose it to UV light for up to 30 minutes, stimulating your collagen fibers to form new bonds.
PKP
PKP (penetrating keratoplasty) or a corneal transplant is only necessary for severe cases of keratoconus. It involves removing your corneal tissue using a femtosecond laser or a round blade and replacing it with healthy donor tissue.
Do you think you may be experiencing symptoms of keratoconus? Schedule an appointment at South Texas Eye Institute in San Antonio, TX, today to stay in the know about the health of your eyes!

